The Insidious and Dangerous Challenge of Crystal Meth
It’s been called a crisis, a scourge, an epidemic, a blight that is corroding the social fabric, destructive to families and individuals. Go ahead, pick your description. When it comes to the use of methamphetamine—or crystal meth—any or all of the above apply.
By Dale Eisler, Senior Policy Fellow, Johnson Shoyama Graduate School of Public PolicyIt’s been called a crisis, a scourge, an epidemic, a blight that is corroding the social fabric, destructive to families and individuals. Go ahead, pick your description. When it comes to the use of methamphetamine—or crystal meth—any or all of the above apply.
It has become a critical issue for people dealing with its consequences. Police across the Prairie Provinces say it is key factor driving crime rates, both violent and property related. Social workers will tell you it is causing significant damage to the lives of individuals and at the root of heartache for many families struggling to cope with its consequences. People in the health care field say it is a growing factor putting additional strain on an already over-stretched system. Worst of all, the trajectory of rising crystal meth usage has been unfolding for years. It is often the symptom of complex underlying economic and social issues that require the coordinated financial and human resources of multiple sources, ranging from social agencies, police, all levels of government, and community organizations. Unfortunately, if you listen to the people on the front lines, that is not happening, at least not to the degree that’s required because the problem keeps getting worse. With Saskatchewan and Manitoba consistently at, or near, the top of national crime statistics, including the crime severity index, a key factor driving the numbers is crystal meth.
Let’s begin with the statistics.
In terms of the total Canadian population, the reported level of crystal meth use appears relatively small. For example, in 2015 a survey by the Canadian Centre on Drug Use and Addiction found that 59,000 Canadians admitted to having used the drug, or about 0.17 per cent of the population. But at the same time, a 590 per cent increase in possession incidents between 2010 and 2017 clearly indicated the availability of methamphetamine has been, and still is, increasing.1 A crucial reason is that relative to other drugs, meth is cheap. A “hit” with what is almost 100 pure meth can cost as little as three dollars.
When you dig into the numbers, and talk to the people on the frontlines of coping with crystal meth and its impacts, a different story begins to emerge. The potent, addictive effects of such an inexpensive drug has spurred huge growth in the illicit drug market. Regina Policy Chief Evan Bray says that crystal meth has become the dominant drug driving issues of gangs and violence. The same is echoed by Saskatoon Police Chief Troy Cooper. “Crystal meth is different than what we face with other drugs. It is so ubiquitous and so present because it is so cheap,” says Cooper. Danny Smyth, Winnipeg’s Chief of Police, echoes those comments, saying that Winnipeg is in the grip of a crystal meth crisis that is getting worse.2 It is the same story in Calgary. “Fentanyl is a community health crisis, meth is a crime and safety issue,” says Chief Constable Steve Barlow of the Calgary Police Service.3
It is also not confined to any particular socio-economic group, but found everywhere in all strata of society. Nor is it exclusively an urban issue. “It’s all over Saskatchewan,” says Dwayne Cameron, an addictions specialist. “I don’t think anyone’s community is immune to it ... we’re seeing it really hit in the rural and First Nations communities.”4 One community struggling with the crystal meth epidemic is the Montreal Lake First Nation, where an estimated 60 per cent of residents are addicted to the drug. “Everybody’s impacted. There’s not one of us who isn’t impacted by having one of our relatives on crystal meth,” says Lionel Bird director of child and family services.5
So what is it about crystal meth that makes it such a growing and dangerous phenomenon?
It’s a synthetic drug that acts as a stimulant on the central nervous system. Here’s how its effects are described by the federal Department of Justice: “Individuals who use methamphetamine will experience increased focus and mental alertness, the elimination of the subjective effects of fatigue, and decreased appetite. Many of these effects are broadly interpreted as euphoria or a sense of well-being, intelligence and power. It is a common belief that methamphetamine gives people ’super-human strength’. Methamphetamine users often become heavily immersed in what they are doing and are prone to violent outbreaks. Other side effects include twitching, jitteriness, repetitive behaviour (known as “tweaking”), and jaw clenching or teeth grinding. Some users exhibit sexually compulsive behaviour and may engage in unprotected sexual encounters with one or more individuals. Chronic methamphetamine use attacks the immune system, and users are often prone to various types of infections. There are also short- and long-term health effects, including paranoia, liver damage, brain damage and depression.”6
The Canadian Centre on Substance Abuse and Addiction says “when methamphetamine is used regularly over a long period, there is an increased risk for developing psychosis or psychotic symptoms. Symptoms include violent behaviour, paranoia, hallucinations and delusions, which pose risks and challenges to medical and healthcare professionals.”
Chart 1: Meth possession and trafficking occurences, Saskatoon
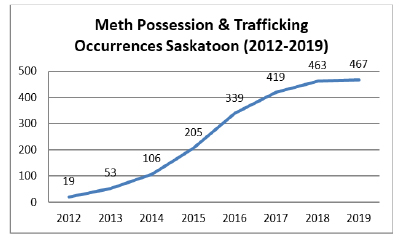
Table 1: Meth seizures, amounts and occurences, Regina
| January to October | |||||
|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | |
| Seizures | 167 | 263 | 320 | 542 | 548 |
| Grams | 932 | 2,144 | 2,839 | 5,751 | 12,184 |
| Occurrences | 84 | 154 | 214 | 347 | 351 |
Source: Regina Police Service
None of that sounds pleasant. So why do people use it? There are many reasons. But, at least initially, one of the prime motives is it’s cheap, easily accessible and people get a quick and powerful rush of euphoria that can last for 12 hours or more. It is that effect which makes it so addictive, and the more a person uses it, the more debilitated they become emotionally and physically. Their judgment becomes skewed as the need for a rush from the drug begins to overtake their lives.
The social and economic consequences
Last June, the all-party House of Commons Standing Committee on Health issued a comprehensive report entitled Impacts of Methamphetamine Abuse in Canada. It portrays a distressing reality based on the committee’s cross-country fact finding. It found “that methamphetamine use poses a unique set of challenges because of its low cost, long-lasting effects, high addiction potential, and the psychic instability it can cause among some users, both in the short and long term.”7 The committee also heard from experts who said that while the use of crystal meth has been increasing nationally, it is happening most acutely in the Western provinces. According to Dr. Matthew Young, Senior Research and Policy Analyst, Canadian Centre on Substance Use and Addiction, the issue needs to be considered in the context of geography and specific groups. “The national survey data tells only a very small part of the story. There is considerable variation in rates of methamphetamine use and problematic use tends to be concentrated among populations that are unrepresented in national surveys,” says Young.
For example, in Manitoba there was a 104 per cent rise in the use of methamphetamine among adults in the past year. At the same time 48 per cent of youth seeking drug treatment for addiction cited crystal meth as the primary drug they were using. Dr. Ginette Poulin, Medical Director, Addictions Foundation of Manitoba, says there has been a massive increase in emergency room visits in the Winnipeg Regional Health Authority and a three- or fourfold increase in deaths associated with methamphetamine use. “One of the challenges, when it comes to addictions, is that it is so multifactorial and layered that we all need to be part of the solution,” says Poulin.
The need for coordinated, multisector engagement is a view shared by many. Chief Bray says the police are trying to cope with the criminal justice effects of the crystal meth issue, which include escalating gang violence and the presence of guns. But that is only one dimension of a much deeper problem. “We need wrap around intensive support that involves health, social services, the police and community groups all working together in a coordinated fashion,” says Bray.
The impact of crystal meth is manifest at multiple levels. It makes policing much more dangerous because the effects of the drug are so powerful and people often are clinically psychotic when under its influence. The result is police face potentially much more volatile situations, often with the growing presence of firearms or other weapons. And the fact the drug’s effects last for so long makes it difficult for police to de-escalate often tense situations. Something as simple as a traffic stop takes on a completely different dimension of potential danger. As a consequence, policing itself becomes more militarized when everyone, including the police, recognize it needs to become less so and more engaged in daily human interactions with members of the community. Instead, the rise of crystal meth is creating growing crisis interventions.
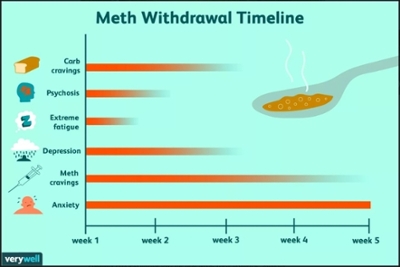
For the health care system, crystal meth has created an entirely new set of medical issues that add new and complicated strains on the system. The lengthy psychotic effects on individuals under the influence of crystal meth makes dealing with them in hospital trauma settings extremely difficult, complex and often dangerous. “It’s really changed the way we have to respond in terms of service available,” explains Tracy Muggli, Director of Mental Health and Addiction Services for the Saskatchewan Health Authority. “People will present in an acute psychotic state and you don’t know if it’s from a mental health episode or from the drug.” As a result, the acute care system becomes the entry point for people exhibiting the effects of crystal meth and have to be held for their own safety and others. Under the influence of the drug people can be very dangerous and need to be kept in “safe spaces” where they can’t harm themselves or frontline health care workers dealing with the situation. Unlike opioids, which act as a depressant to the central nervous system, methamphetamine is a stimulant that often leads to aggression, paranoia and psychosis. If used over a long period of time, crystal meth can result in permanent psychosis. Adding to the health challenge is currently the lack of a drug that can be used to treat the active effects of methamphetamine or addiction to it.
The causes
Reciting the effects and consequences of the drug puts the scope of the challenge into perspective. But beyond treating the symptoms, the key policy issue is how to address the causes.
People who deal with the impact of crystal meth, whether it’s health care officials, law enforcement, social service agencies or community groups, all agree there are multiple socio-economic reasons people turn to the drug. Without question, a major factor is its cheap price and availability. But beyond the accessibility issue, the key reason is that something, or things, are wrong in the lives of people who become addicted to the drug. It is often a combination of many factors. It can be the result of other underlying mental health issues. But very often there are socio-economic reasons such as unemployment and poverty, homelessness, sexual assault, other forms of abuse, family dysfunction, or the long-term effects of residential school experience on Indigenous people. The bottom line is that people in at-risk communities are especially vulnerable to becoming drawn into the crystal meth web as they try to cope with the reality of their lives. The rapid and powerful effects of crystal meth, which give people a sense of euphoria and mental acuity, provides an escape from the challenges that people face. In effect, it alters an individual’s emotional reality by stimulating their senses in a way that provides relief from the circumstances of their lives. But citing the social factors driving the crystal meth numbers does not mean that people are absolved of personal responsibility for their actions. Ultimately it is about choices individuals make about how to deal with their circumstances.
Identifying the solutions
In its report on the impacts of methamphetamine abuse in Canada, the House of Commons Standing Committee on Health said collaboration between federal, provincial and territorial governments in the context of the Canadian Drug and Substances Strategy would be an important first step. It pointed to the need for public education; building resiliency in youth, parents and communities; greater access to harm reduction; investments in withdrawal management, treatment and psychiatric care; better access to housing and social supports; and, re-evaluation of criminalization of simple possession of illicit psychoactive substances. By outlining the litany of needs, the committee report demonstrates the breadth of the challenge and the necessity for collaboration.
The good news is, in some respects, that kind of multi-pronged approach is already happening. Three years ago, the Crystal Meth Working Group (CMWG) was initiated by Mental Health & Addiction Services within the Saskatchewan Health Authority to address the challenges experienced in providing service to those struggling with crystal meth use. The work has generated basic educational information about crystal meth for front-line workers as well as identification of evidence-based treatment approaches and methods to provide worker safety, which form the basis of staff training. It involves front-line Mental Health and Addiction Services staff and focuses on four main areas: Prevention; Treatment Challenges and Transitions; Withdrawal Management; and, Safety. The same kind of collaborative work is the impetus behind The Regina Intersectoral Partnerships, as well as the Safe Community Action Alliance in Saskatoon (a collaborative of 35 community individuals/agencies), both of which deal with the impacts of drug abuse on communities and individuals. One potential benefit of a single health authority for the province is having the governance structure to ensure that all the relevant agencies and stakeholders are working in a co-ordinated fashion. However, to date there is no clear evidence that’s happening. Rather, as suggested by one engaged in the crystal meth issue, it is through the “sheer determination” of those working in the field and other community members who know something needs to be done that coordination is occurring.
Last October, community partners endorsed the work of the Safe Community Action Alliance (Crystal Meth working group) and proposed four initial actions. They were to establish a drug court in Saskatoon; create crystal meth and fentanyl-specific treatment option; create more 24/7 safe spaces for youth; and, establish more coordinated outreach services.8 Shortly after the proposed measures were announced the provincial government signalled a drug court would be established in Saskatoon. As well, in its 2019 Budget, the Saskatchewan government committed $30 million in additional funding for mental health and addictions. It represented what Health Minister Jim Reiter said was “the largest commitment ever to mental health services in our province.”9 But how much of the additional funding is going to the crystal meth issue is unclear.
Diagram 2: Hierarchy of needs in addictions recovery

Conclusion
There is reason for some degree of optimism in the fact that progress has been made in mobilizing people and resources to meet the societal challenge presented by the rise of crystal meth. But given the complexity of the socio-economic issues involved much more needs to be done. The most important next step is political leadership that begins at the highest levels of government, which is crucial to raise broad public awareness of the issue. It needs to be recognized for what it is, a major health care, law enforcement, public safety and social challenge that requires a public commitment of the resources, people and expertise to address it. With that must be the public recognition that there is no easy solution. But because it’s so difficult is no reason not to act in a way that people on the frontlines say we must. It’s time for people with power, influence and the ability to make a difference, to step up and meet the challenge.
References
2 https://aptnnews.ca/2019/07/22/police-stats-showcase-the-impact-of-winnipegs-meth-problem/
3 https://www.ourcommons.ca/DocumentViewer/en/42-1/HESA/report-26/page-84
4 https://globalnews.ca/news/5128644/crystal-meth-saskatchewan/
5 https://www.cbc.ca/news/canada/saskatchewan/mlcn-tactics-combat-crystal-meth-use-1.5432328
6 https://www.justice.gc.ca/eng/rp-pr/other-autre/meth/p3.html
7 https://www.ourcommons.ca/Content/Committee/421/HESA/Reports/RP10533589/hesarp26/hesarp26-e.pdf
8 https://safecommunityactionalliance.com/
9 https://www.cbc.ca/news/canada/saskatchewan/sask-budget-mental-health-2019-20-1.5064518Dale Eisler

Prior to joining the JSGS, Dale Eisler spent 16 years with the Government of Canada in a series of senior positions, including as Assistant Deputy Minister Natural Resources Canada; Consul General for Canada in Denver, Colorado; Assistant Secretary to Cabinet at the Privy Council Office in Ottawa; and, Assistant Deputy Minister with the Department of Finance. In 2013, he received the Government of Canada’s Joan Atkinson Award for Public Service Excellence. Prior to joining the federal government, Dale spent 25 years as a journalist. He holds a degree in political science from the University of Saskatchewan, Regina Campus and an MA in political studies from Vermont College. He also studied as a Southam Fellow at the University of Toronto, and is the author of three books.